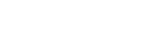
Factors Contributing to the Formation of Pressure Ulcers
First off, what is a pressure ulcer (also known as bedsores, decubitus ulcers, and decubiti)? It is a lesion or wound that occurs when the skin is exposed to a prolonged period of pressure, shear force and/or friction. These pressure ulcers start from small lesions on the skin to gaping holes where muscles, tissues, and bone can be seen, leading to a painful death (click here to learn about the stages of pressure ulcers). Prevention will help avoid major pain and discomfort, disfigurement, improve the quality of life of the patient, and decrease health care expenses. Although the factors below may sound like something only the elderly will experience, it can also occur in our youth - being temporarily immobile for months due to an accident, or when a neurological condition is present whereby there is a loss of sensation, for example.
It is important to note that pressure ulcers must not be mistaken with moisture lesions as they require different types of care. Click here to learn the differences between the two.
Now, let us get into it - intrinsic and extrinsic factors that may lead to the formation of pressure ulcers.
INTRINSIC FACTORS

Immobility
Immobility can be seen as the root cause of pressure ulcers as pressure ulcers are rarely seen on mobile and active individuals. The reason being is, as mentioned, pressure ulcers will form when there is constant load or pressure on the skin. That load and pressure cut off blood circulation leading to tissue damage and broken skin. They can form while sitting or lying down for extended periods of time. Common places that they may form are over bony areas of the body - back of the head and ears, shoulders, elbows, hips, lower back, buttocks, inner knees, and heels. They can also form when medical equipment presses on the skin - oxygen tubing presses against ears or cheeks.
Sensory Loss / Neurological conditions
On top of immobility, sensory loss is another factor that requires attention when it comes to the formation of pressure ulcers. Our skin and nerves send signals to the brain to tell it if the body is experiencing any pain or discomfort. If that ability is lost, the body can no longer know when it is in pain and the body doesn’t shift when necessary, leading to increased risk of developing pressure ulcers.

Aging
Skin aging is the bane of most women’s adult life. We know that aging causes the skin to thin, lose elasticity, lose collagen, and decrease in the strength of the skin. We spend thousands of dollars on creams, lotions, and facial treatments. But did you know, that for the bedridden, those skin aging facts can be fatal? Aging skin tears easily while the patient is being transported or even when there is a slight shift of the skin. For example, friction between the skin and bedsheets. Environmental factors (which we will get into later in) also play a part in causing the skin to be compromised and increase the risk of developing pressure ulcers.
Chronic Illness
Especially illnesses such as Diabetes and vascular disease which affect blood flow are especially high risk at developing bedsores. One of the things that our skin requires to keep healthy is good blood circulation. Chronic illnesses like Diabetes, for example, will build up plaque in the blood vessel due to damage caused by high glucose levels in the blood.
EXTRINSIC FACTORS
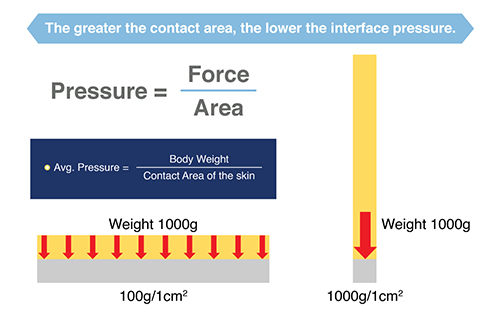
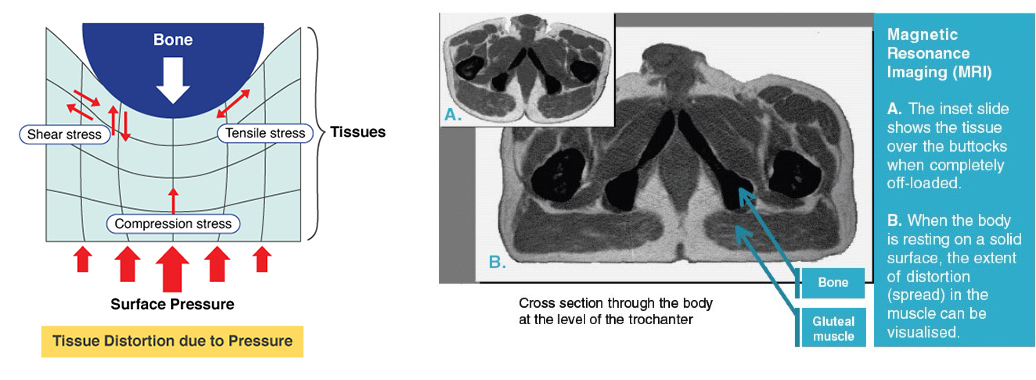
Pressure
Pressure on the skin can limit blood flow and contribute to bedsores by not allowing vital oxygen and nutrients to be delivered to the skin and surrounding tissues. Why is that? Well, just like the human body, if our bodies lack the nutrients it needs to survive, eventually, we will succumb to disease and pass on. The same goes for our skin. The lack of nutrients to the skin and tissues will lead to tissue and skin damage that may eventually die and turn into pressure ulcers.

Incontinence
Regardless if it is urine or fecal incontinence, there will always be water and moisture being expelled from the body. Cleaning must be done right after every urination and bowel movement to prevent the skin barrier from breaking down over time and turning into pressure ulcers. Click here to learn about proper cleaning and skincare for those with incontinence.

Humidity & Heat
As written under ‘incontinence’, excessive moisture on the skin increases the risk of developing pressure ulcers as it weakens the skin barrier and becomes more susceptible to tears from friction or shear force (which we will cover below). Now, the same applies to humidity. Heat and humidity in the air can cause perspiration on the body. Parts of the body to pay particular attention to are the back of the neck, elbows, underarms, back of the knee, the groin area just to name a few. Generally, anywhere that would be easier for sweat to develop and accumulate.
Friction and shear force
Before we head into how friction and shear force can cause pressure ulcers, let’s first get the definitions of both squared away.
Friction: When two surfaces in contact, slide in opposing motions (example: clothes rubbing against skin, or rubbing your palms together creates friction)
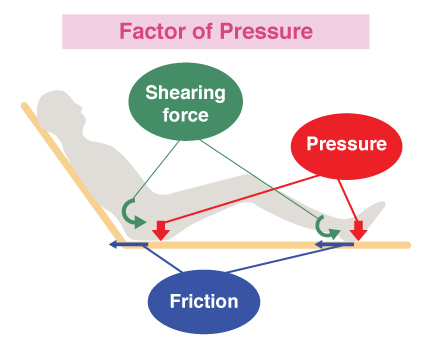
Shear force: When one part of the body/skin is being stretched in a specific direction while the other part of the body/skin is stretched in the opposite direction (example: stretching your skin in opposite directions is creating shear force)
Friction, shear force and pressure all work together to develop pressure ulcers. Friction and shear force ‘tightens’ or ‘thins out’ the skin making it more susceptible to tears and ulcers when pressure is applied. If you ever notice pressure ulcers forming, please consult your doctor immediately to manage and mitigate the severity.